The NHS is not underfunded
Inefficiency, not underfunding, is at the root of its ills
Earlier this month, the OECD published its annual Health at a Glance report. It does not contain anything fundamentally novel: the OECD runs a huge database of healthcare-related indicators, which it keeps updating continuously as new data comes in, and the report just provides some commentary around the data.
The UK is now comfortably in the global top 10 in terms of healthcare spenders
The UK is now comfortably in the global top 10 in terms of healthcare spenders. In 2022, the UK spent 11.3 per cent of GDP on healthcare, ahead of, for example, Belgium (10.9 per cent), the Netherlands (10.2 per cent) and Australia (9.6 per cent), about on a par with Switzerland, and surpassed only by the United States, Japan, France, Germany, and Austria. This goes against the conventional wisdom that the NHS is “chronically underfunded”, and that “underfunding” is the source of all of its problems.
It is true that if we look at healthcare spending in cash terms rather than as a proportion of GDP, the UK drops out of the top 10. This is because, even though we still — wrongly — think of Britain as a rich country, by OECD standards, Britain is not “rich” at all. Healthcare spending may be 11.3 per cent of GDP in both Britain and Switzerland, but 11.3 per cent of Switzerland’s GDP per capita is a lot more than 11.3 per cent of Britain’s GDP per capita.
However, there is a good reason why healthcare spending is usually reported in per cent of GDP rather than in cash terms. Healthcare is a very labour-intensive sector (which is one reason why it is so hard to squeeze any productivity improvements out of it), so the bulk of healthcare spending is staff costs. These tend to rise broadly in line with GDP per capita. Thus, a given sum of money buys you a lot less healthcare in Switzerland than it does in Britain, and adjusting for differences in the general price level only goes so far in correcting for that.
Every healthcare system in the world is “underfunded”, in the sense that there is no system in which a healthcare provider would not know what to do with an additional £1,000. But “underfunding” is not the reason why the NHS fails to provide the standards of healthcare that health systems of comparable countries do manage to provide.
For example, the OECD report shows that in 2021, there have been 71 avoidable deaths from treatable causes for every 100,000 people in the UK. That is a bit better than Greece and Chile, where the corresponding figure is 76 avoidable treatable deaths per 100,000 people, but worse than, for example, Germany (66), Israel (58), Belgium and Austria (57), France and Norway (51), Japan (49), the Netherlands (48), Australia (47) and Switzerland (39).
UK data on waiting times has not been updated for a while, and waiting times data is only available for a small number of countries. Even so: if we compare the UK’s pre-Covid waiting times to Dutch waiting times today, it turns out that the latter are usually at least a quarter shorter than the former.
While the NHS extends healthcare coverage to 100 per cent of the population, the OECD report shows that the same can be said about the systems of Australia, Canada, the Czech Republic, Denmark, Finland, Greece, Iceland, Ireland, Israel, Italy, Japan, South Korea, Latvia, Luxembourg, New Zealand, Norway, Portugal, Slovenia, Spain, Sweden, Switzerland, Austria, France, Germany, and the Netherlands. Several other countries fall just short of 100 per cent, but this has probably more to do with exemptions for short-term residents and/or cross-border workers than with people being unable to afford health insurance. Universal coverage is great, but it is not a special achievement.
While the NHS is not, in an obvious sense, underfunded, one can make the case that it is understaffed and underresourced. Britain does have fewer doctors, nurses, hospital beds, MRI scanners and CT scanners than most of its peers. But this should not be seen as some external constraint, for which the NHS cannot be blamed. Rather, the question we should ask is why the NHS is worse at converting a pile of cash into manpower and medical equipment than other health systems. A part of what makes a good system “good” is its ability to procure the equipment it needs, and even more so, to recruit, motivate, and retain the staff it needs. If the NHS cannot do that, then that is very much part of the problem.
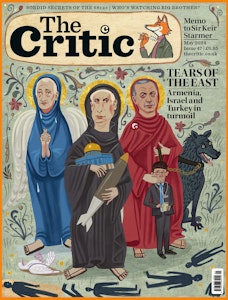
Enjoying The Critic online? It's even better in print
Try five issues of Britain’s newest magazine for £10
Subscribe