Endometriosis meets gender ideology
The real problem is not the appointment of a transgender woman as CEO of an endometriosis charity
Endometriosis is a condition experienced by millions of women and girls globally; an oft-cited statistic is that one in ten have the condition. Given that it takes on average 7.5 years to receive a diagnosis in the UK, even when women and girls are in crippling pain that destroys their quality of life, the rate may well be higher.
Yet there is an utter dearth of knowledge about the disease. Not only is there no known cause of the condition, but its pathogenesis — what actually occurs at a cellular level and why — is unknown. We do know that cells similar to the lining of the womb appear elsewhere in the female body, particularly in the pelvic region but not necessarily. These cells break down in response to hormonal changes, causing internal bleeding. This in turn leads to scar tissue that can cause organs to fuse together. There are multiple theories as to how such cells appear outside the womb in the first place, however. An early theory, still prominent, is known as “retrograde menstruation”, but this fails to explain how endometrial tissue can appear in (for example) the lungs and brain, or why it has been found in foetuses.
There is no known cure, just a scattering of treatments, ranging from medication to surgery, designed to alleviate symptoms which range from infertility to excruciating pain. Because the progression of the disease is poorly understood, these medical interventions are unreliable and can be dramatic, with relief from symptoms being short-lived. Induced menopause using gonadotropin-releasing hormone agonists (also used as puberty blockers) or through oophorectomy (ovary removal) is one treatment. There is also no non-invasive test for endometriosis — a heritable component is likely, but no specific gene has been identified — and its presence can only be confirmed through laparoscopic surgery and laboratory testing. The struggle to be heard, diagnosed and treated, is widespread. First person testimonies of the illness are usually bleak, and suicidal thoughts are common.
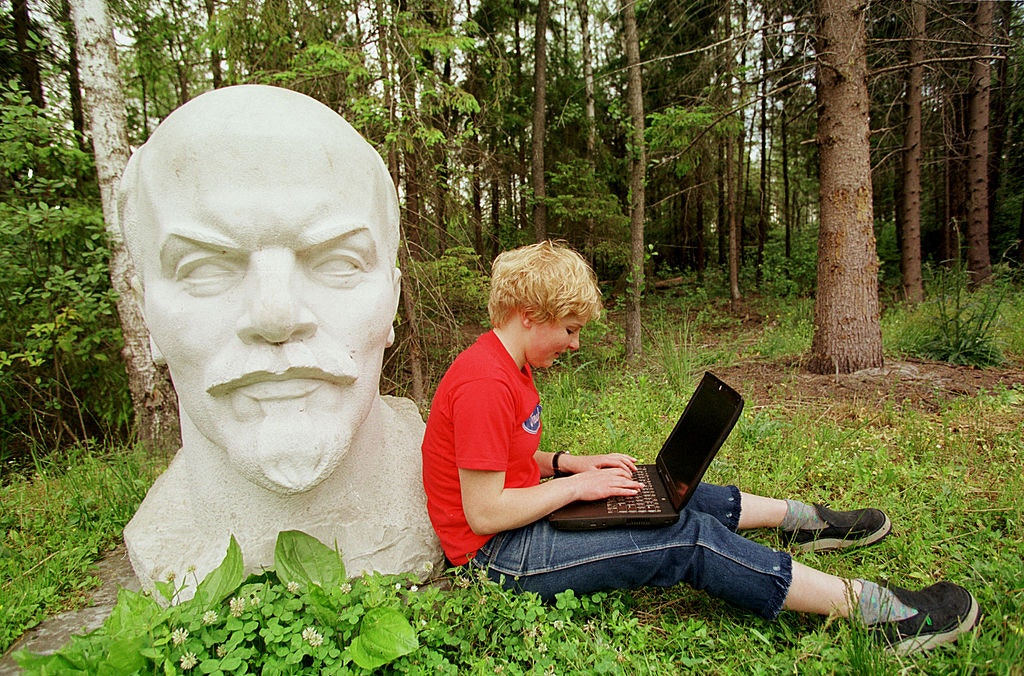
Medical information sites use all manner of bizarre wording, many contradictory and unscientific
Amongst all the confusion, however, there is one thing we do know: endometriosis is a female-specific disease. Given the shared histories of medicine and misogyny, this fact is very probably responsible for all the above unknowns.
Perhaps unsurprisingly, the recent appointment of Steph Richards, a transgender woman, to the position of CEO of the charity Endometriosis South Coast, caused a social media storm. Richards, being a trans woman, is male, and hence cannot get endometriosis. The appointment made a lot of people, especially women, very angry. My own rage centred around the charity’s celebratory post on Twitter/X that featured the following quote next to a picture of Richards: “Isn’t it ridiculous that I’ve got to my 40s, before any medical professionals even mentioned endometriosis?”
However, Endometriosis South Coast later clarified that the quote was not from Richards (who, by the way, is 71) but from one of the women who had benefited from its support. The charity was founded by endometriosis sufferer Jodie Hughes, who is a single mother and PhD student in the subject of endometriosis care. Hughes stated on BBC Radio 4’s Woman’s Hour on 15 November, when interviewed along with Richards, “The CEO of Prostate Cancer UK is a female. They can’t get prostate cancer. A CEO doesn’t need to have endometriosis. A CEO doesn’t need to be that sex.” I agree, particularly as Endometriosis South Coast is a tiny charity with a yearly income of £8,000, staffed entirely by volunteers with full-time other jobs who all suffer from the condition. See also the work of the late Sir David Amess MP, who launched the All-Party Parliamentary Group on Endometriosis and chaired it until his death.
Many women’s concerns lie elsewhere, however. For a start, there is Richards’ previous campaigning, such as organising a protest against the FiLiA conference in Portsmouth in 2021, but this is a separate — albeit significant — problem to that discussed here. Perhaps the primary worry expressed is that Richards will influence the charity with some kind of gender ideology agenda. As Emma Barnett told Richards on Woman’s Hour, “There is a concern that you will not preserve the importance of things like the word ‘woman’ and that experience, because in your statement on X ‘10 per cent of those assigned female at birth suffer from this disease’”.
This worry is misdirected for two reasons. Firstly, since its inception, Endometriosis South Coast has focused on welcoming those with endometriosis however they identify. It was this aspect of the charity’s work that led Hughes and Richards to meet, at an inclusivity awards ceremony. The lack of mention of the word “woman” on the charity’s Twitter/X page reflects an pre-existing ethos that actually informed the appointment of Richards, rather than the other way round.
Secondly, and more importantly, omitting the word “woman” is already a global phenomenon when it comes to endometriosis information and organisations. It certainly is not limited to this charity — in fact, the reference by Hughes to “sex” on Woman’s Hour is actually unusual. The websites of all major endometriosis organisations, and many medical information sites, use all manner of bizarre wording, many of which contradict each other and are unscientific. Some, like the Mayo Clinic, avoid mentioning the affected demographic completely, even in response to the question “Who gets it?”. Others use the dehumanising terms “menstruators” (Mass General Brigham) and “anyone with a uterus” (Planned Parenthood) instead of women and girls. Still others, in complete contrast, repeatedly stress that menstruation or uterus-having is not necessary for the condition. It is true that the condition can continue after a hysterectomy and is indeed not always linked to menstruation, but this is often bizarrely conflated with the idea that it is not, therefore, a female condition. The website for the US Endometriosis Summit states, mind-bendingly, “We recognize that not everyone with endometriosis or a gynecological disease is female. As the disease is found in locations all over the body and all bodies with the disease are not the same, menstruation is not synonymous with endometriosis.”
Endometriosis is glaringly, blindingly, a female condition
Richards, really, is just a distraction. A greater issue is that a debilitating illness, about which we already know very little, that affects millions of women and girls globally, is now being obscured by scientific inaccuracy. We can no longer speak clearly about who it affects. This problem cannot be resolved simply by continuing to use the words “women and girls” to refer to female people. In this essay, I am doing just that, for want of a better option, but I don’t like doing so. This is not because I worry about hurting people with my language — I do, particularly if it alienates those I most want my arguments to reach, but when scientific reporting is inaccurate, people get hurt in other ways, and that is what this story is about — but because I want to use language that everyone understands. “People assigned female at birth” is laughable — see this study on endometriosis in female foetuses. The problem is that for some people, “women” means those who refer to themselves as women. For others, it means female adults, however they refer to themselves. If half the people reading what I have written infer something else, then I as a writer have failed. My goal is to maximise the number of people who understand me. “Female people” in place of “women and girls” would solve this problem, but that brings other issues, and anyway would be rejected by both the Emma Barnett camp and the Jodie Hughes camp. Ultimately, I want to be accurate not just on my own terms but on everybody’s terms. Today, that feels impossible.
In March, I encountered two articles on the popular US website Healthline, which prides itself on its medical accuracy. The stories focused on male endometriosis. The title of one, “Can Men Have Endometriosis? 11 Things to Know”, naturally led me to believe the subject of the article would be transgender men.
But, no. Even though there have been important studies into trans men with endometriosis, one suggesting a rate as high as 25 per cent — studies which are essential, and could also help us understand the condition better, particularly given the use of hormone treatments and hysterectomies — the article largely focuses on “cisgender men and other AMAB folks”. Sixteen recorded cases of male endometriosis, rather than being seen as extraordinary anomalies that might illuminate our understanding of endometriosis in general, which is what the scientific reports of those cases suggest, are instead used to support various conclusions that make a mockery of those with the condition — transgender men included. According to Healthline, males with unexplained lower back pain should mention endometriosis to their doctor, and males suffering from low sperm motility should “be sure” to raise endometriosis as a possible cause. The latter claim links to a study that does indeed suggest that endometriosis reduces sperm motility, but not in the way Healthline claims: endometrial tissue growing in women can reduce the motility of sperm travelling through their body after sex. For Healthline, however, experts “need more research” to understand “how endometriosis specifically can affect male reproductive organs”. Ultimately, “given how rare it is for AMAB individuals to have endometriosis, it can be tricky to get an endometriosis diagnosis”. Don’t take no for an answer, lads!
The other article, called, “How common is endometriosis?” (it has since been deleted, but is archived here) considers the same historic male cases to be proof that endometriosis is “not sex-specific”, though it is acknowledged that “the rates vary greatly based on a person’s sex assigned at birth”, a genuine contender for the most understated claim of all time. It concludes by saying, “Endometriosis doesn’t discriminate based on sex, gender, genitals, genetics, or anything else. In other words, anyone can develop endometriosis.” When I sent the article to evolutionary biologist Jerry Coyne, who had emailed me in response to my essay about New Scientist’s habit of misrepresenting scientific papers, he replied: “Shoot me now! They say 16 men had endometriosis, though some of those probably lived in the past. If we assume they all live in the present, then the frequency of endometriosis in men is 0.000000002. BUT ANY MAN CAN GET IT. And any man can be hit by lightning — the chances are 32,300 times greater of getting zapped during your lifetime than of getting endometriosis. Your chance of being hit by lightning TWICE is still greater than getting endometriosis.”
So there we have it. Endometriosis is glaringly, blindingly, a female condition. It is also one that exposes that there is more to being female than simply female sex organs. As a result, attempting to discuss it in gender-friendly language seems to cause some kind of system malfunction. It just isn’t possible, and it leads to ridiculous and contradictory consequences. Worse still, the resulting confusion adds another layer of obscurity to what we know about the condition. If the prospects for understanding endometriosis anytime soon were poor, now they are dismal.
When the default body is considered to be male, women and girls suffer
Part of the problem is that gender ideology identifies genitalia and breasts as the sole physical expressions of manhood and womanhood (when it isn’t arguing that gender is completely unrelated to the physical body). This is almost identical to the “bikini approach”, a term coined by renowned cardiologist Nanette Wenger to expose the faulty perception within the medical field that sex differences only exist in the areas covered by a bikini. She has worked to expose the harms of bikini medicine for decades, and she is now 93. Scientific studies still fail to disaggregate data by sex (Caroline Criado Perez is the expert on this). When the default body is considered to be male, women and girls suffer as a result. When it claims that sex differences are limited to reproductive organs, gender ideology is actually mirroring medical misogyny. Every cell in the body is different depending on whether the individual is male or female, and this is not irrelevant trivia. It is essential to understanding female health and making scientific progress.
In the Woman’s Hour interview, Jodie Hughes said of endometriosis, “It’s not a reproductive disorder — it being seen as a gynaecological disorder maybe is the reason why for the last 200 years, research and medicine isn’t progressing.” Emma Barnett replied, “So we’ve got to rebrand something that men can have to be taken seriously?” Hughes is now being roundly criticised for these comments, but perhaps she was actually referring to crucial studies exposing the flaws in the retrograde menstruation theory. The interview then ended, so I don’t know. Sadly, what was not discussed was that Barnett and Hughes both have endometriosis, which has had enormous impacts on both their lives. Hughes lost her career as a chef and then went to university, with no GCSEs. She wrote a dissertation about stress levels in women with endometriosis, after which she completed an MA with an expanded thesis on 1,000 women worldwide. She is now working on her PhD. She had a hysterectomy at 32. Meanwhile, Barnett had extended cycles of IWF and multiple miscarriages as a result of endometriosis, before having two children. Whilst on maternity leave she wrote a book about period shame; for her, as with many women, agonisingly painful periods have been a dominant endometriosis symptom.
The experiences of these two women could have been the topic of their conversation. Like Hughes, Barnett cares about the struggles of trans men and those who identify as non-binary; she devotes a section to their experiences in her book. I don’t believe their perspectives are so different. Barnett is concerned about the loss of the word “women”, but Hughes may not wholly disagree; she uses “women” in the section on the charity’s website where her academic work is mentioned. In fact, the word “woman” is present on her charity’s site more than on any other website — charitable or medical — that I mention in this piece. Instead, a combination of linguistic challenges, coupled with conflicting theories around endometriosis and the diverting subject of Richards, meant that the conversation ended in confusion and conflict. Earlier, Barnett had asked, “Do you regret this appointment?” to which Hughes replied, “Absolutely not.” Barnett continued, “even though it has led to a conversation like we have been having, as opposed to about endometriosis?” Hughes then said, “I’m really, really devastated that I’m not on here talking about endometriosis and my PhD work.” Barnett said that Hughes would be able to “come back and do that”. I really hope that happens.
Because it affects so many people and affects them so very badly, but remains barely understood, the case of endometriosis exposes the misogyny at the heart of medicine and science. It underscores just how little we understand about the female body. The condition is utterly incompatible with a gender narrative that minimises sex differences and jumps on the misogynistic “bikini” bandwagon, rather than resisting it. Endless claims that “anyone can have endometriosis” keep us trapped in a world in which the specifics of women’s health are ignored.
On Woman’s Hour, Richards said, “I was brought into Endometriosis South Coast to raise the awareness of endometriosis full stop, and also to raise the profile of Endometriosis South Coast. It’s pretty amazing that in five days, I’ve achieved that, and the vehicle that’s done that is transphobia.” Obviously, I would dispute that the questions I have raised here are “transphobic”, since I don’t believe facts are hateful, or that anyone benefits from a false narrative that minimises sex differences in medicine. In a way, though, Richards has a point. Were it not for Jodie Hughes’ decision, I would never have binge read medical journals on endometriosis, nor stayed up until 3am reading Emma Barnett’s book, nor lain awake thinking about what a sad, sad world we live in. Just when we were starting to make progress on the understanding of female health, a flawed belief system came along that took us back to square one and denied us the language we need to communicate clearly.
Enjoying The Critic online? It's even better in print
Try five issues of Britain’s newest magazine for £10
Subscribe